OVERVIEW
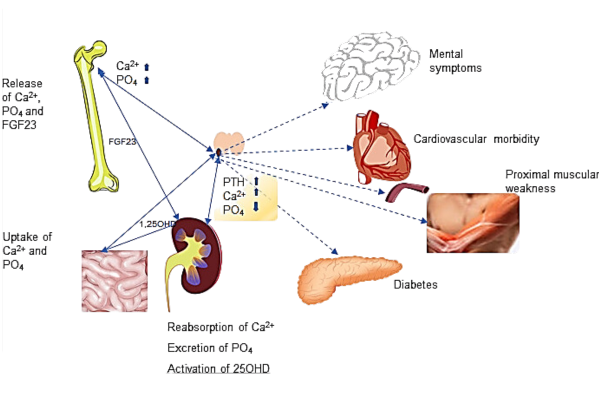
Primary Hyperparathyroidism (PHPT) is third most common endocrine disorder after diabetes mellitus and thyroid disorders. The prevalence of primary hyperparathyroidism varies from 1 in 400 to 1 in 1000 persons in western populations. The clinical manifestations of primary hyperparathyroidism ranges from asymptomatic hypercalcemia detected during routine testing to classic manifestations traditionally associated with disease. Fuller Albright in 1930 described pentad of primary hyperparathyroidism which includes bone pains, renal stones, abdominal groans, psychic moans and fatigue overtones. The PHPT is biochemically characterized by inappropriately elevated parathyroid hormone (PTH) in the presence of hypercalcemia. It is also associated with low serum phosphate and elevated alkaline phosphatase. Primary hyperparathyroidism is also associated with increased urinary calcium and phosphate excretion.
RISK FACTORS
You may be at an increased risk of PHPT if you:
- Are a woman who has gone through menopause
- Have had prolonged, severe calcium or vitamin D deficiency
- Have a rare, inherited disorder, such as multiple endocrine neoplasia, type I, which usually affects multiple glands
- Have had radiation treatment for cancer that has exposed your neck to radiation
- Have taken lithium, a drug most often used to treat bipolar disorder
Cause
PHPT occurs because of some problem with one or more of the four parathyroid glands:
- A noncancerous growth (adenoma) on a gland is the most common cause (85%).
- Enlargement (hyperplasia) of two or more parathyroid glands accounts for most other cases (10-15%).
- A cancerous (malignant) tumor is a rare cause (1%).
Primary hyperparathyroidism is usually nonfamilial, but some people inherit a gene that causes the disorder.
symptoms
Symptoms may be so mild to severe and nonspecific that they don’t seem at all related to parathyroid function. The range of signs and symptoms include:
- Fragile bones that easily fracture (osteoporosis)
- Bone and joint pain
- Kidney stones
- Excessive urination
- Abdominal pain
- Tiring easily or weakness
- Depression or forgetfulness
- Frequent complaints of illness with no apparent cause
- Nausea, vomiting or loss of appetite
TREATMENT
Surgical removal of adenomatous gland is the first line of the treatment for PHPT.
Complications
Complications of hyperparathyroidism are primarily related to the long-term effect of too little calcium in your bones and too much calcium circulating in your bloodstream. Common complications include:
- Osteoporosis: The loss of calcium often results in osteoporosis, or weak, brittle bones that fracture easily.
- Kidney stones: The excess of calcium in your blood may cause small, hard deposits of calcium and other substances to form in your kidneys. A kidney stone usually causes significant pain as it passes through the urinary tract.
- Cardiovascular disease: Although the exact cause-and-effect link is unclear, high calcium levels are associated with cardiovascular conditions, such as high blood pressure (hypertension) and certain types of heart disease.
Neonatal hyperparathyroidism: Severe, untreated hyperparathyroidism in pregnant women may cause dangerously low levels of calcium in newborns.
Diagnosis
After the clinical evaluations, the diagnosis of PHPT is made by blood tests.Serum calcium levels are elevated, and the parathyroid hormone level is abnormally high compared with an expected low level in response to the high calcium. Biochemical confirmation of primary hyperparathyroidism is following by investigations to localize the enlarged gland. Tc99 sestamibi scan of head, neck and upper thorax is the most commonly used test for localizing parathyroid adenomas. Ultrasonography is also a useful test in localizing suspicious parathyroid lesions.